Read our papers for more details: Saez et al., 2021; Mutti et al 2023
Read our first Capsid & Tail issue here.
In our past paper in 2021, we talked about how plaquing host range of phages does not correlate with their efficacy in liquid cultures or biofilms and the need to adapt phagograms.
By breeding phages, we increased their lytic capacity by 99% over their ancestors, allowing the creation of a phage cocktail with a coverage of 92% of the 110 strains of our panel. However, even liquid cultures did not reflect the reality of in vivo infections. Getting experiments closer to physiological conditions, it was observed that all anti-staphylococcal phages were losing their activity when we added plasma or synovial fluid in our growth media.
Digging into literature, there were hints from an article in 1965 by Bartell et al., they found that in S. aureus infected mice, when the bacteria and the phage treatment were administered simultaneously, mice survived. However, the survival rate diminished when the treatment was delayed by 30 minutes after the bacterial infection.
Yet, we wanted to go further: if we could get to the details, we might be able to solve it.
Why are S. aureus phages inactive in plasma?
We observed that the activity of anti-staphylococcal phages was already inhibited in 0.5% plasma or synovial fluid. Although phage replication occurred, bacterial lysis lagged, resulting in no substantial reduction in bacterial population. This happened for all tested aureus phages across genetically very different families.
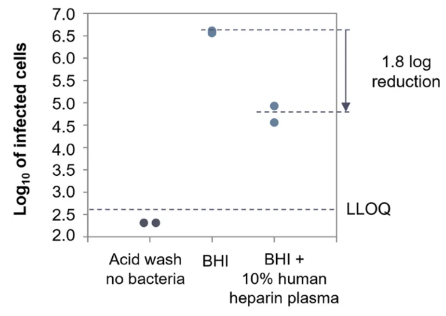
S. aureus is well known for binding coagulation factors, in two processes named clotting and clumping, i.e. forming aggregates. We thought these may be shielding the bacterium from phages. In fact, as you can see in the publication, phages are not able to adsorb to the bacterium (Figure 1).
Figure 1. ECOI of Herelleviridae phage PM93, in human heparin plasma. The log 10 of the number of infected cells (cell suspension at 5 × 108 CFU/ml infected with 5 × 106 PFU/ml) is plotted against the different conditions tested in the assay.
By using isolated blood components and proved that purified fibrinogen significantly hindered phage activity, at a concentration below the one in human blood.
Translating these findings to a mouse S. aureus thigh infection model, we found that phage treatment did not reduce bacterial burdens, indicating that in vivo, the bacteria might be protected from the phages as well.
Why is phage training not enough? Is there a solution?
We tried to breed our phages by adapting the Appleman´s protocol, directing their evolution towards the infection of aureus in plasma. However, the genetic change needed to disrupt the clots formed by aureus apparently needs a bigger change than what can be achieved with this method. In fact, this inhibition in plasma happened in all families of phages tested and was already described by other groups for different phages, strongly indicating that all anti-staphylococcal phages may be impacted.
Further investigation revealed that dissolving clots with tissue plasminogen activator (tPA), an anticoagulant, partially restored phage efficacy. However, using an anticoagulant implies risk of hemorrhage. This hints for the use of a local anticoagulant delivered by an engineered phage, which could act exclusively on the clot, and may have potential to solve this problem.
What are the implications?
Phage activity of S. aureus phages is severely diminished in blood and synovial fluid: this means that for certain infections such as PJIs, chronic wound infections, osteomyelitis, soft tissue abscesses, and endocarditis, it is an imperative to further research this phenomenon to ensure the efficacy of phage therapy.
What’s next?
Based on these data, we abandoned phage research back in 2021. With this publication we hope to help other research groups move forward and solve this problem.
Read our papers for more details: Saez et al., 2021; Mutti et al 2023
Read our first Capsid & Tail issue: “ɛ²-phages: naturally bred high-tech phages which are superior to wild types in critical properties” here.