I’ll take you on a journey of how phage therapy has had an impact on my life within the past year. The fall of 2018 was the first time I’d ever heard of this therapy as a possibility for treating the terrible lung infections that plague me.
I’ve had a bacteria called Pseudomonas aeruginosa festering in my lungs for as long as I can remember. I was born with a progressive genetic disease called cystic fibrosis. It is characterized by the buildup of thick sticky mucus primarily in the lungs but also affects the digestive tract and sinuses. The cycle of bacterial lung infections caused by this trapped mucus building up over time requires repeated antibiotics to treat them, mostly intravenously. The concurrent inflammation from the immune system trying to fight the infection leads to lung damage and eventually respiratory failure, shortening the life of a person with the disease, if a lung transplant does not occur to hopefully prolong life.
Over the past few years, these infections have become more frequent, so much so that it’s gotten to a point where I require oral antibiotics almost constantly, as well as higher doses of antibiotics delivered intravenously three or more times a year. Yet, the antibiotics’ ability to kill off the bacteria is waning.
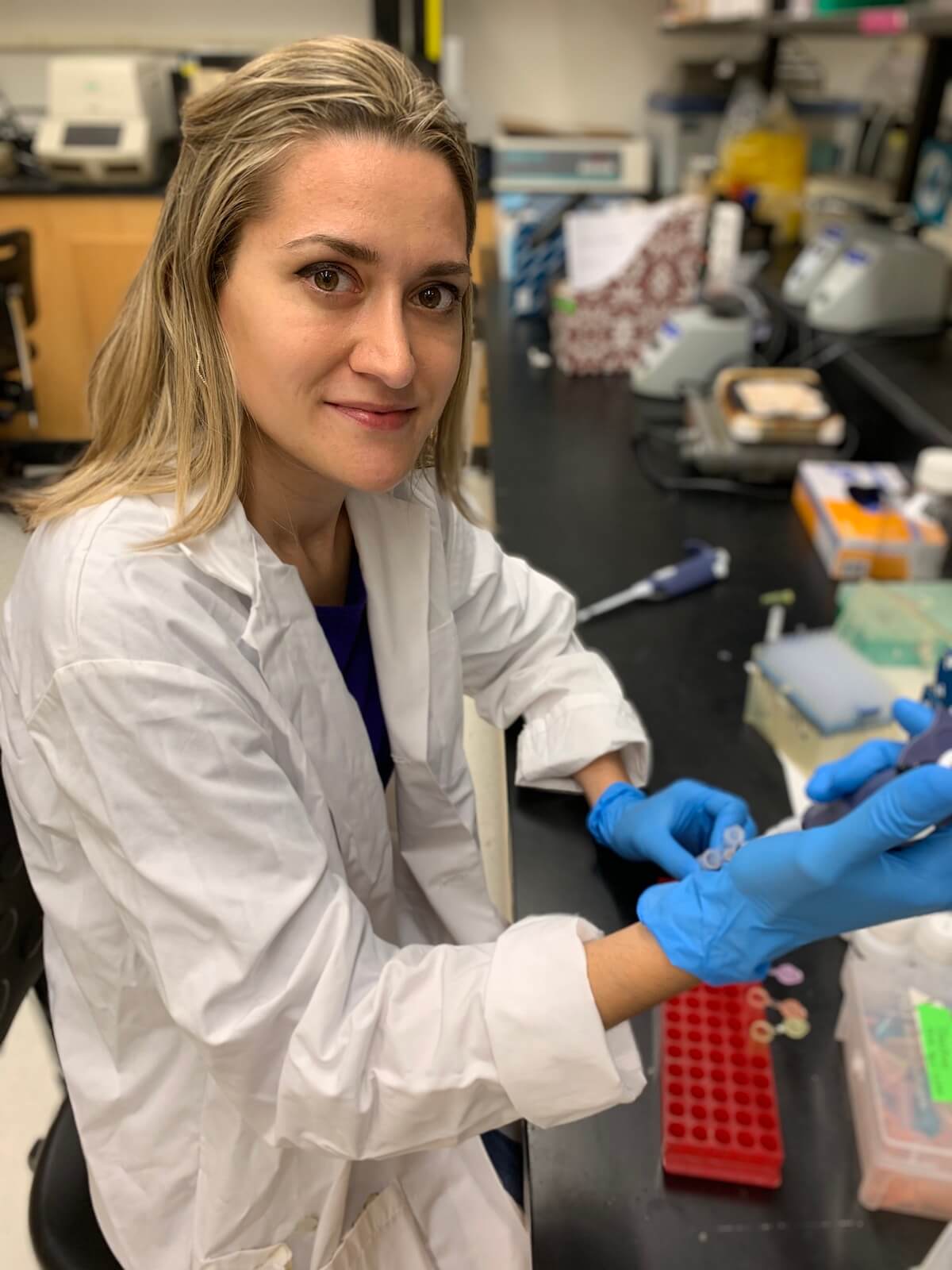
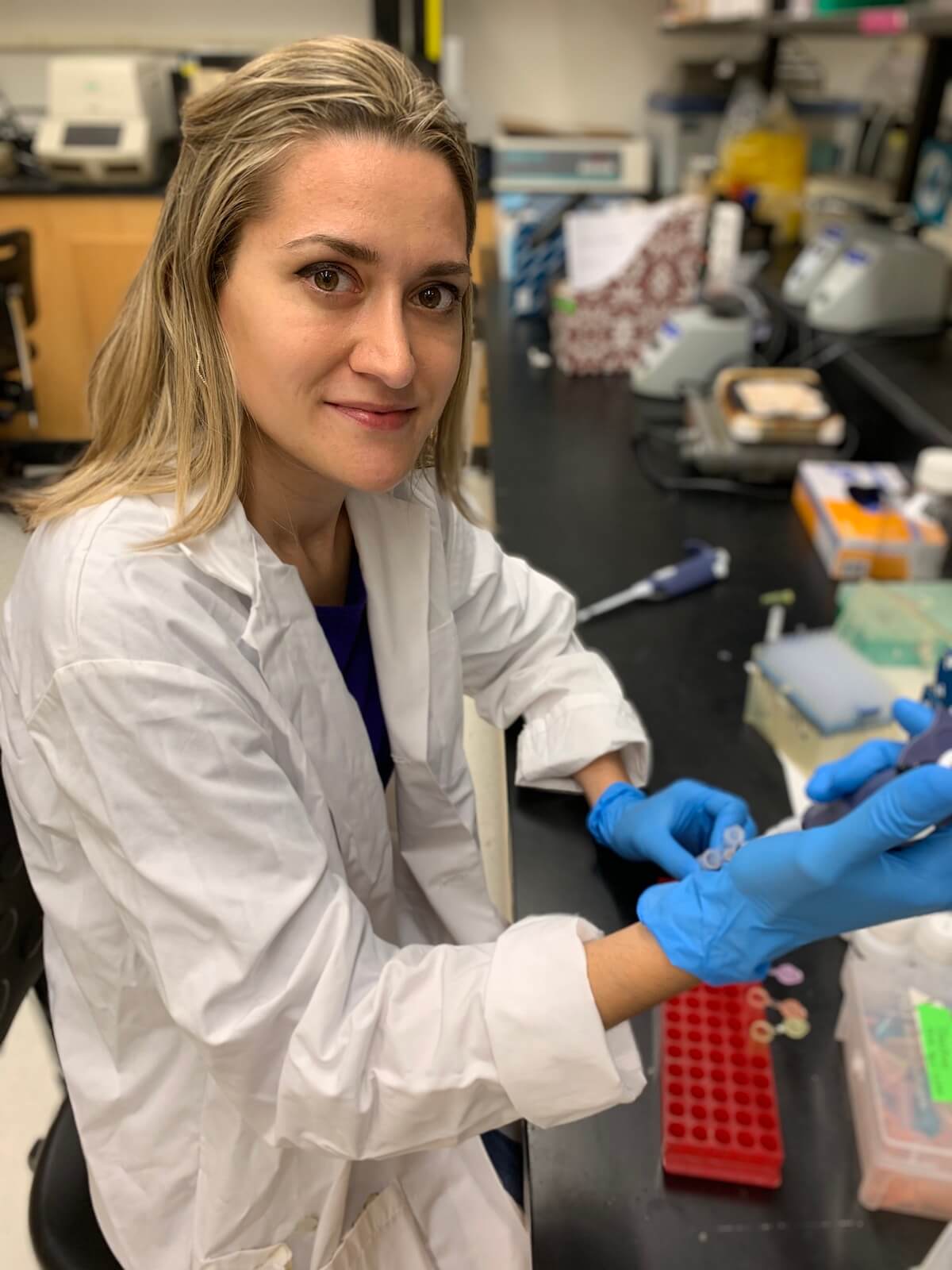
Ella Balasa performing DNA extractions at Virginia Commonwealth University.
I am a microbiology lab technician and a freelance writer. In 2018, I was contacted by a company that was doing a documentary about a CF patient who was treated with phage by Yale University researchers. They asked me to write a synopsis of what living with CF is like to accompany the video. This was the first time I had heard of phage therapy and I was amazed. I knew I needed to contact the researchers to try this therapy for myself. That was how my journey began.
At the time, I was on the brink of the worse infection I’ve ever had, with my lung function reaching a mere 18% by the time I was treated in January 2019. To read details about my treatment from my perspective, click here.
In short, about a week after phage administration the Pseudomonas infection began to clear. The use of phage simultaneously with IV antibiotics changed the bacteria’s sensitivities and facilitated a synergistic attack on them — one they couldn’t repel. I stayed antibiotic free for about 6 months after that — a significant amount of time thus far in the trajectory of my lung disease.
In this time, I began advocating for phage therapy and serving as a voice to other patients. It was propelled by the Associated Press documentation of my treatment, and I also wanted to share my story personally to bring awareness to this potential treatment option for the CF community and beyond it.
With my science background, I’ve had an interest in learning about the fascinating way phage can be manipulated to provide the best outcomes with treatment. I’ve had many patients who are interested in accessing phage therapy reach out to me asking for advice and guidance. I share what I know about the biological aspects of phage, what I have learned about the process of obtaining treatment, the work there is still to be done with the FDA, beginning clinical trials, and just public awareness about the benefits of this treatment in general. In April, I connected with Diane and Mark Smith, who have supported IPATH and Yale researchers in memory of their daughter, Mallory, to advance phage research as quickly as possible.

A book tour at UVA for Salt in My Soul. Mallory Smith’s parents, Mark and Diane (left), Ella Balasa (center), Terri Quinan (CF Foundation), and assistant (right). Used with permission.
In the past few months I’ve attended conferences during which phage therapy was a top focus of sessions. At one of these conferences, not only did I see the Yale researchers who treated me, but I also met a researcher who knew of me only as patient “EB”, and seeing me in person, was awestruck. This was a researcher who had heard of my treatment case earlier this year when I was treated with the same phage he was presenting information about on his poster. I was also amazed by the connection between researcher and patient coming full circle, and the privilege to be contributing to research so directly.

Ella Balasa attending Infectious Disease Week Conference in Washington DC, October 2019.
Another wonderful connection and opportunity happened at the very university where I work. Unbeknownst to me, there are phage researchers teaching the SEA-PHAGES program at Virginia Commonwealth University (VCU), and, learning of my case and my interest in phage research, asked me to speak to the class and offered to teach me how to isolate my own phage from water and soil samples. So far, we may have isolated a temperate phage.
Earlier in the year, I joined the CF Foundation (CFF)’s Infection Research Committee, and have advocated for phage therapy to be at the forefront of the research agenda in the future. I wrote a blog with the Director of Drug Discovery at the CFF detailing the science of phage to the CF patient population. More recently, I have spoken at the Milken Institute to raise awareness about the dire problem we face against antibiotic resistant bacteria and the need for development of novel therapies outside of traditional antibiotics to treat them.
Most recently, I have been asked to speak of my experience at the Phage Futures 2020 Conference. Advocating for phage therapy will continue to be a focus of my efforts until it is a standard of care treatment for all patients combating antibiotic resistant infections.
I also hope to be able to benefit from phage treatment again in the near future as I know Pseudomonas will get the upper hand over me once more.
Ella will be speaking about her experience receiving and advocating for phage therapy at the Phage Futures Congress in Washington, DC next week (Feb 5-6). For a 10% discount off your registration, enter code PHAGEDIRECTORY.